When Your Child Needs Chest Physical Therapy (CPT)
Chest physical therapy (CPT) is a method for clearing mucus out of the lungs. Keeping the lungs clear helps your child breathe easier. CPT involves three main steps:
When to do CPT with your child
Do CPT with your child 1 to 4 times a day for no more than 20 to 40 minutes at a time. If your child has a respiratory infection, you may need to do CPT more often. Talk about the schedule with your child’s healthcare provider or physical or respiratory therapist. It may be helpful for more than one person to know the method. This can help you stay on schedule. In general, do CPT:
-
First thing in the morning and right before bedtime
-
When your child’s stomach is empty, either before meals or at least 1 and a half to 2 hours after meals
-
Before or after breathing treatments as instructed by the healthcare provider
-
After exercise, which helps loosen mucus. Check with the healthcare provider first about this.
Position your child
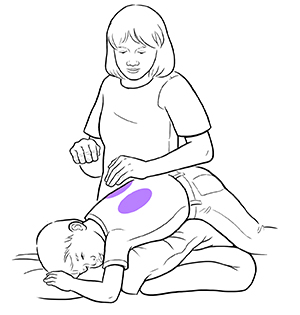 |
| CPT is done in different areas of your child’s chest, back, and shoulders. A physical or respiratory therapist can teach you the exact positions and techniques to use with your child. |
Special positions help you use gravity to drain mucus from your child’s lungs. This is sometimes called postural drainage. Have a box of tissues handy for when your child coughs up mucus. A healthcare provider will show you positions to use with your child. Positions may depend partly on your child’s age. For example, you can place a small child in your lap. You can have an older child lie on a flat surface, such as a bed or floor. In either case, when your child is lying down, have the child’s head and chest lower than their hips. You can use pillows or a foam wedge to create this position.
But don't use this position with a baby. And don't use it if your child has problems with GERD (gastroesophageal reflux disease). GERD is an ongoing (chronic) condition in which stomach acid backs up into the esophagus. Talk about the best position with the healthcare provider if your child has been diagnosed with GERD.
Clap on your child
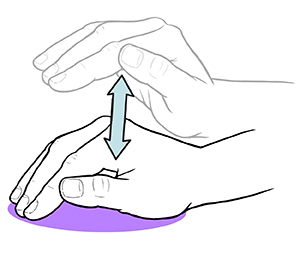 |
| Correct hand position for clapping. |
Once your child is positioned, you can start clapping to loosen secretions in the lungs. Remove any rings, watches, or bracelets before you start. Have your child remove necklaces and clothing with buttons or zippers around the chest or neck. They can wear light, comfortable clothing, like a T-shirt. Here are steps for clapping:
-
If your child is not wearing a shirt, put a thin cloth or sheet on their body. Don't do percussion directly on skin.
-
Cup your hand to trap air between the hand and your child’s body. Keep your thumb next to your index finger.
-
Clap against your child’s rib cage. Move your wrist, not your arm and shoulder. Clap on the left side of the rib cage, then the right side. Be careful not to clap on the stomach area, breastbone, lower ribs, or spine.
-
Keep clapping firmly and steadily but not too hard. Do this for about 3 to 5 minutes in each area.
You can also use other airway clearance devices, such as a vest, to get a similar effect. The vest is attached to an air generator that causes gentle, continuous vibration. The motion vibrates the chest to loosen mucus. Oscillating positive expiratory pressure (PEP) is another method. With PEP, your child may use one of a variety of devices to blow air all the way out, while the device creates air waves to help break up the thick mucus. You can ask your child’s healthcare provider or physical or respiratory therapist about these options.
Have your child cough
Coughing clears mucus out of the lungs. If your child is older, have them cough after you clap on each area. Don’t start clapping again until your child has stopped coughing. To get your child to cough, have your child do this:
-
Sit up and bend forward a little.
-
Take a breath.
-
Open the mouth and tighten stomach muscles to cough deeply, not just from the throat.
-
Spit any mucus that is coughed up into a tissue.
-
Take another breath.
-
Repeat until lungs are clear.
Making it easier for your child to cooperate with CPT
You can do many things to make CPT easier for your child. With experience, your child may feel better and come to enjoy this time with you.
-
Think of ways to help your child relax and take control. When possible, have your child choose the position to start in.
-
Explain in simple ways how the methods help.
-
Have your child choose a fun activity to do during CPT, such as listening to music or watching a video.
-
Praise your child for cooperating.
Possible side effects of CPT
Some children have side effects of CPT. Most are mild and go away soon after stopping CPT. Make sure a small baby is positioned so that you can check breathing and the color of the face. Call your child's healthcare provider for help if side effects continue after trying the strategies above. Here are possible side effects of CPT:
-
Unrelieved coughing. Stop CPT. Start again only when your child can breathe easily.
-
Upset stomach (nausea). Have your child rest for a while. If your child vomits, end that CPT session. Make sure you do CPT when your child’s stomach is empty. Encourage your child to spit out the mucus, not swallow it.
-
Pain. Stop CPT. Make sure your hand is cupped, not flat.
-
Trouble breathing. Stop CPT. Have your child sit up. When breathing is back to normal, start CPT again.
-
Crying. Distract your child by giving them something to do. Small children have trouble lying still.
-
Dizziness. Stop CPT for a while and let your child relax. Start again when dizziness is gone.
-
Gastroesophageal reflux. This is when stomach acid backs up into the esophagus. If this happens, don't put your child in a head down position.